Implant Placement Lateral to the Inferior Alveolar Nerve: Selective Indications and Treatment Outcomes—A Case Series
Georges Tawil, DDS, DSc, OD; Peter Tawil, DDS, MSc; and Ziad Salameh, DDS, PhD
Abstract: Replacement of missing posterior mandibular teeth in severely atrophied jaws can be quite challenging. Various treatment options have been proposed for the rehabilitation of the deficient posterior mandible with implant-supported prostheses. Depending on the clinical situation, it may be feasible to place implants lateral to the inferior alveolar nerve, which represents a viable treatment option under the proper circumstances. This article defines the indications and limitations of this approach and presents the treatment planning and surgical management of three selected cases and their outcomes 1 to 5 years after implant loading.
Implant placement in the resorbed posterior portion of the mandible can be highly challenging for a variety of reasons. Among them are limited bone quantity consequent to horizontal or vertical ridge resorption, occlusal considerations that result from increased interarch distance, poor jaw-to-jaw relationship, absence of buccal vestibule, absence of ridge height in relation to the floor of the mouth and interference with muscle function, absence of a stable band of keratinized gingiva, and resultant difficult access for oral hygiene.
Several treatment options have been proposed for the rehabilitation of the deficient posterior mandible with implant-supported prostheses. Vertical and/or horizontal reconstructive approaches using autogenous graft from intra- or extraoral sources and guided bone regeneration using autogenous bone combined or not with bone substitutes and resorbable or nonresorbable membranes are well-documented with consistent results,1-5 although various complications can be expected depending on the clinician's expertise, technical difficulties that may arise, and patient risk factors. Inferior alveolar nerve (IAN) repositioning, distraction osteogenesis, or segmented osteotomies with interpositional bone grafting can be valid options in well-indicated situations.6-10 The use of short (≤8 mm) implants has proven to be a suitable alternative to advanced surgical treatment with good long-term results.11,12 Ultrashort implants (<5 mm) also have been used successfully, but long-term results are still needed to validate this approach.13
Some clinical situations may allow for implants to be placed lateral to the IAN, which also represents a viable treatment option. The purpose of this case series is to define the indications and limitations of this option and present treatment planning and surgical management of three selected cases and their outcomes 1 to 5 years after implant loading.
Case 1
The patient, a 65-year-old woman with no systemic conditions and who was under no medications at the time of consultation, presented for the replacement of her mandibular right molars. She reported that 4 months before consulting with the authors, two implants were placed in the mandibular right quadrant in sites Nos. 30 and 31. The implant placed in site No. 30 failed and the No. 31 implant was still osseointegrating but was positioned too lingually and would be difficult to use as a support for a fixed dental prosthesis because of the severe buccolingual discrepancy with the opposite dentition. Offset occlusal loading with consequent biomechanical complications, food impaction, and difficult access to oral hygiene precluded the use of implant No.31 in a future prosthetic rehabilitation.
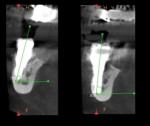
Full clinical examination revealed a stable periodontal condition with no pockets of more than 5 mm, bleeding on probing of less than 15%, no significant tooth mobility, and no mucogingival problems. A mandibular jaw cone-beam computed tomography (CBCT) scan showed a 6 mm to 8 mm bone height coronal to the IAN but a 5 mm to 7 mm buccolingual discrepancy between the mandibular ridge and the opposite dentition (Figure 1). The IAN was positioned lingually with 5.2 mm to 6.2 mm distance to the external cortical plate. A digital impression (TRIOS® 3, 3Shape, 3shape.com) was done and the file exported along with the CBCT data to a 3D software planning program (TRIOS Implant Studio® on dental desktop version 1645, 3Shape) for complete evaluation and treatment planning (Figure 2). Prosthetic crowns were positioned ideally in relation to the opposing jaw, and the implants were placed crown down in the alveolar housing. In this particular case, ideal implant positions in relation to the opposing arch were buccal to the alveolar nerve, though emerging in a zone of alveolar mucosa.
Treatment options were as follows: either place the implants in the available alveolar bone and reconstruct the case prosthetically after osseointegration, with a severe buccolingual discrepancy and potential biological and biomechanical complications; or reconstruct the bone horizontally to match the opposing dentition, place implants 4 to 6 months after bone grafting, and complete the case prosthetically, an option that would be quite demanding technically, time-consuming, and relatively costly; or place the implants buccal to the IAN, which is a delicate technique that requires high precision in surgical handling but is effective and fast. The creation of a stable zone of attached gingiva buccally would need to be re-evaluated in all scenarios and properly handled. A sufficient distance between the IAN position and the external cortical plate would allow the placement of a 10 mm x 3.3 mm implant with a 1.5 mm safety zone.
All options were discussed with the patient, including an orthodontic treatment to realign the maxillary ridge and treatment of the compromised prosthetic with an offset prosthetic reconstruction. It was decided that the opimal treatment option in this case was to place the implants buccal to the IAN. The aforementioned Implant Studio software was used for digital 3D CT-based surgical planning. The implants were virtually placed according to bone anatomy and prosthetic planning. A stereolithographic toothborne surgical template was ordered based on the software analysis and that would allow for the use of the necessary drills for implant placement.
For the surgical procedure, the patient was premedicated with midazolam 7.5 mg 1 hour before the procedure. Local anesthesia (Septanest 4% with 1/100,000 epinephrine, Septodont, septodont.co.uk) was administered in the buccal and lingual vestibules. It was decided to open a flap because of the concomitant explantation of the implant placed in site No. 31. A horizontal incision was made on the alveolar ridge and two vertical releasing incisions were done mesial to the first bicuspid and distal to the second molar. The flap was elevated buccally and lingually. A 5 mm trephine was used to remove the implant placed in site No. 31. Then the surgical guide was positioned on the remaining mandibular teeth (Figure 3). An initiating drill to a depth of 4 mm to 5 mm followed by a 2.2 mm twist drill and, finally, a 2.8 mm twist drill were used to prepare the implant bed. Countersinking and bone tapping completed the preparation.
A 10 mm x 3.3 mm bone-level implant (Straumann® Bone Level Roxolid®, Straumann, straumann.com) was initially placed in site No. 31. However, because of a poor primary stability due to an unnecessary tapping, it was removed and placed instead in site No. 30 with an excellent primary stability. A 10 mm x 3.5 mm implant (NobelReplace® Conical Connection NP, Nobel Biocare, nobelbiocare.com) was then placed in site No. 31 with a good primary stability (Figure 4). Healing abutments were connected, and the flaps were sutured with 4-0 vicryl sutures.
Two months later, implant integration was confirmed (Figure 5). A digital impression was taken and two CAD/CAM zirconia splinted crowns were fabricated and cemented on the implants (Figure 6 and Figure 7). One year later, the implants' emergence in a zone of alveolar mucosa was evaluated. Peri-implant soft and hard tissues were stable with no signs of inflammation, and oral hygiene was good. It was decided to keep the patient under observation for the potential need to create a zone of keratinized gingiva.
Case 2
A 53-year-old female patient with no systemic conditions presented for full-mouth rehabilitation. Following the rehabilitation of the maxilla by a fixed restoration supported by eight implants and the mandibular left posterior area by implants in sites Nos. 20 and 21 and crowns on Nos. 19 through 21, the mandibular right sextant needed to be addressed. CBCT imaging revealed a very limited bone volume coronal to the IAN (Figure 8), which was an indication for vertical reconstruction followed by the placement of three implants and a four-unit fixed restoration after allowing several months for graft maturation.
The patient, who had already gone through some long, strenuous, and elaborate treatment, asked if a less invasive procedure could be done to address the mandibular right region. Analysis of the CBCT revealed a lingual positioning of the IAN that was 6 mm distance from the external cortical plate, allowing placement of two 10 mm x 3.75 mm implants. At site No. 28, a 10 mm Brånemark System RP implant (Nobel Biocare) could be safely placed in sufficient bone volume and height. A prosthetic evaluation was done using a 3D software planning program (NobelClinician®, Nobel Biocare), which confirmed the possibility of implant placement lateral to the IAN with an adequate subsequent prosthetic rehabilitation. A surgical guide was produced based on the prosthetic analysis, and the implants were placed according to the surgical and prosthetic planning. The surgical guide was used to determine implant position with an initiating drill. Subsequent drilling was done freehand.
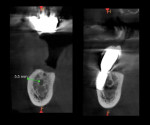
A 2 mm twist drill was used first at the predetermined distance from the external cortical plate and oriented 10 degrees toward the opposite arch. Corono-apical movement of the drilling was done, with the drill orientation being maintained and the external cortical plate always being leaned on. A drilling guide was placed to confirm the bur's orientation. This was followed by the use of a 3 mm twist drill and bone countersinking. Two 10 mm x 3.75 mm Brånemark RP machine-surfaced implants were placed with excellent primary stability in sites Nos. 30 and 31, and 3 mm healing abutments were connected (Figure 9). Two months of healing were allowed.
Exposure of the healing abutments was performed via a split thickness vestibular deepening procedure, and a periodontal dressing was placed to stabilize the soft tissues apically. Multi-unit abutments were connected along with two plastic healing caps. Four weeks later, final impressions were taken and a four-unit fixed dental prosthesis was connected articulating with the fixed maxillary restoration in an anticipated cross-bite occlusion (Figure 10). The maxillary teeth could have been reset prosthetically but the patient was happy with her function and esthetics. The occlusion as set, hence, was accepted.
Five years post-loading, the mucogingival environment around the implants emerging in the vestibular alveolar mucosa was stable (Figure 11). Soft and hard tissues showed excellent stability, and at the time of this writing there was no need to perform a gingival graft to create a zone of stable keratinized peri-implant gingiva.
Case 3
The patient, a 75-year-old woman, presented for the replacement of her missing posterior mandibular teeth following the failure of a long-span bridge extending from the third molar to the second bicuspid and that served 15 years in function. Recurrent decay on both supporting teeth, Nos. 29 and 32, indicated their extraction. Clinical and radiographic analysis revealed a limited amount of bone coronal to the IAN due to natural bone remodeling following tooth loss and the coronal intrabony course of the IAN. Sites Nos. 29 and 30 could be used for the placement of regular-platform implants: an 11.5 mm x 4.3 mm Select conical implant in site No. 29 and a 7 mm x 4 mm Brånemark RP implant in site No. 30 (Nobel Biocare). Limited bone volume remained in sites Nos. 31 and 32 based on CBCT analysis (Figure 12). The lingually positioned IAN at the level of the third molar at 5.5 mm from the external cortical plate left room for the placement of a 3.3 mm diameter implant.
Treatment options were discussed with the patient, including vertical reconstruction followed by implant placement or implant placement lateral to the IAN. The patient agreed to the latter option. A digital mandibular impression was taken and the digital imaging and communications in medicine (DICOM) file was transferred with the CBCT via an implant planning program (NobelClinician) for surgical and prosthetic evaluation. It was decided to place an 8 mm x 3.3 mm implant (Straumann Roxolid) in site No. 32 buccal to the IAN. A surgical guide was designed to enable determination of the initial entry point of the bur and its angulation. The rest of the drilling was done freehand because of the difficult surgical access. Drilling was continued, leaning on the external cortical plate during drilling and maintaining the direction of drilling (Figure 13), and an implant was placed with an excellent primary stability. A 1.5 mm buccal dehiscence was treated with autogenous bone grafting and a resorbable collagen fleece (Figure 14).
Three months later, implant-abutment connections were made and a fixed cemented dental prosthesis was placed with the anticipated limited cross-bite occlusion at the level of the second molar (Figure 15). Three years later, the implant-supported restoration was very stable with a well-maintained peri-implant bone level as confirmed by CBCT (Figure 16).
Discussion
Replacement of missing posterior mandibular teeth in severely atrophied jaws can be quite challenging. Several case scenarios can be identified that may favor the conservative treatment modality option of placing implants lateral to the inferior alveolar nerve. Cases, such as in Case 1, may present where bone coronal to the IAN allows implant placement but presents a severe buccolingual discrepancy with the opposing ridge. In such a case, the prosthetic reconstruction with a severe off-axis positioning of teeth may often result in biomechanical complications, food entrapment spaces, difficult access for oral hygiene, and patient dissatisfaction. Treatment options may include either horizontal reconstruction of the ridge followed by implant placement or orthodontic management to properly align the maxillary arches. Patient age, treatment duration, morbidity, and cost may preclude acceptance and compliance, especially in elderly patients. The second case scenario (Case 2), a more common situation, is one with a severe bone resorption and a limited residual bone volume coronal to the IAN, thus precluding the use of even short implants and indicating vertical bone reconstruction prior to implant placement.
Finally, as seen in Case 3, cases may present where bone volume coronal to the IAN is limited although ridge height is within what usually would be a manageable range for implant placement if not for the IAN location in the superior part of the mandibular body, an anatomical variant that has been found in 30.7% of cases and limits bone availability for implant placement.14 In that situation, crestal bone resorption is limited but the intrabony course of the IAN seriously restricts implant placement without well-defined vertical bone augmentation preceding implant placement.
In all of these types of cases, if the IAN course in the mandibular body is lingual, allowing the placement of implants buccally, this treatment option, although a sensitive technique with little margin for error, can be indicated. In such cases, a clinical and radiographic investigation must be done to determine the possibility of implant placement lateral to the IAN with an acceptable prosthetic end-result. It is suggested that this type of procedure be done only by experienced clinicians.
Surgical management is delicate. Limited bone volume for implant placement lateral to the IAN necessitates precise prosthetic planning and surgical management. The entry point in bone is the most critical part of the drilling sequence and must be determined based on the presurgical prosthetic planning and fabrication of a surgical guide. An initial drilling to 4 mm to 5 mm depth is followed by use of a 2 mm twist drill. Drill orientation and site preparation depth are then checked. Drilling is completed with the surgeon leaning on the external cortical plate to avoid the bur slipping in the less dense marrow bone. The 1.5 mm safety zone is critical in the corono-apical direction because of the bur end shape and the inevitable overextension of the drilling to reach the appropriate site depth. It is more precise to operate in the buccolingual direction where the drilling is done to the actual size of the bur. This explains why it is possible to approach the IAN to within a distance of less than 1.5 mm and remain safe. However, if site preparation is imprecise, damage to the IAN may occur.
Daróz in a CBCT analysis of 30 mandibles found that 3.75 mm diameter implants could be placed lateral to the IAN in 28.7% of the cases.15 If the IAN is at least 5.5 mm distance from the external cortical plate, and the prosthetic planning favors the treatment based on analysis of the end-result, placement of the implant lateral to the IAN may be a valid option. Stereolithographic or surgical guides can be designed to assist in implant placement. Several clinical and in vitro studies compared their efficacy in partially and totally edentulous patients and in cases of toothborne or mucosa-borne templates.16,17 Although CAD/CAM guides proved to be more precise than surgical guides in the lateral direction and more consistent in their deviation between the planned and actual implant location,18 errors still have been reported in angulation as well as coronal and apical deviations.19 The lowest and highest mean error at the entry point was 0.15 mm and 1.7 mm, respectively. The mean apical deviation varied between 0.28 mm and 2.99 mm, and the mean angular deviation ranged from 1.49 to 8.54 degrees.20 Vertical displacement was found to be consistent in the apical direction, meaning that implants were always placed deeper than originally planned.18
A 2 mm safety zone from anatomical structures must be maintained to compensate for the possibility of errors.20 Bone-supported guides showed significantly larger deviations than tooth- or mucosa-borne guides. Among the complications reported using CAD/CAM guides was the lack of primary implant stability during placement. This occurred in 1.3% of the cases and must be properly handled to avoid implant loss.20 In a comparison of computer-guided versus freehand implant placement in fully and partially edentulous patients, no statistically significant differences were found between the two approaches in terms of implant failure, complications, peri-implant marginal bone level, surgical time, or prosthetic time needed to complete the treatment except for more postoperative pain and swelling in the freehand-treated group.21
A stereolithographic guide was used in one of the present cases, while in the other two cases a surgical guide served to determine the initial drilling point. Thereafter, the implants were placed freehand, with the surgeon leaning on the external cortical plate during drilling, maintaining the direction during the corono-apical movement and the buccolingual angulation of the drill as determined during planning. This approach is highly delicate and requires flawless control of the drilling. It proved to be very effective in these cases, as no interference with the adjacent vital structures occurred in any of the cases. For less experienced clinicians, surgical guides are safer and should be preferred. However, access to the surgical site can be difficult, especially in posterior areas of the mouth in cases of limited mouth opening. Implant placement using dynamic navigation has been introduced in recent years.22 Freehand surgery with real-time 3D guidance of the drill allows implant positioning with high accuracy with an entry error of 0.4 mm and an angular deviation approximating 4 degrees without the need of surgical guides after a learning curve is achieved.23 The application of this technology, however, is dependent on the availability of somewhat sophisticated hardware in the dental setting.
The need for a stable zone of keratinized gingiva around implants has been widely debated in the literature. The absence of a stable zone of attached gingiva has been associated with a significant increase in peri-implant bone loss.24 Up to 1.35 mm of bone loss might be expected if implants are placed in thin mucosal tissues.25 Thickening of thin tissues with membrane reduced crestal bone loss from 1.81 mm to 0.44 mm after 1 year.26 It was suggested that more tissue height is needed for biologic width to protect the underlying bone.26
Other studies did not support these findings, however.27,28 Greater soft-tissue recession on buccal sites was found when the width of keratinized mucosa was <2 mm (compared to sites with >2 mm) without jeopardizing implant survival in rehabilitated completely edentulous patients at 5 years.29 Bengazi et al observed lack of an attached portion of masticatory mucosa at 61% of all implants with no consequences on peri-implant soft-tissue health.30 Bouri et al examined the significance of attached gingiva in subjects with dental implants and found higher plaque index scores around implants with a narrow zone of attached gingiva (<2 mm) compared to implants with a wide zone of attached gingiva (>2 mm).31 Subjects reported an inability to brush these areas due to mucosal mobility and tenderness.
Lastly, a 1.8 mm osseous thickness around dental implants was thought to be the minimum thickness for adequate vasculature for osteocyte nutrition and function.32 This figure, however, is based on clinical observations rather than scientific studies.
It is important to note that in the current case series, the postoperative remodeling of a thick and dense cortical bone, as found in the external oblique ridge area, may result in minimal marginal bone loss and obviate the need for a thick peri-implant attached gingiva, provided the access to oral hygiene is assured and proper maintenance is possible. CBCTs taken 2 to 6 years post-treatment confirmed crestal bone stability and soft-tissue health in these cases. However, this concept needs to be substantiated in well-conducted comparative clinical trials.
Conclusion
This case series presented three clinical scenarios for implant placement lateral to the IAN. Presurgical prosthetic planning with appropriate software is imperative for this treatment, as it will allow the clinician to determine the feasibility of implant placement, avoid surgical complications such as potential bleeding issues or nerve damage, and anticipate the prosthetic end-result. Successful outcome depends on proper case planning and surgical and prosthetic execution. With proper access to oral hygiene and maintenance, the minimal thickness of a very dense buccal cortical plate and the absence of a stable peri-implant attached mucosa seem compatible with a stable result in this highly particular clinical context. This, however, remains to be confirmed by long-term, well-conducted clinical trials.
About the Authors
Georges Tawil, DDS, DSc, OD
Professor Emeritus, St. Joseph University, Beirut, Lebanon; Private Practice, Beirut Dental Specialists Clinic, Beirut, Lebanon
Peter Tawil, DDS, MSc
Private Practice, Beirut Dental Specialists Clinic, Beirut, Lebanon; Member, American Board of Periodontology
Ziad Salameh, DDS, PhD
Professor, Director of the Research Center, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon
References
1. Peñarrocha-Oltra D, Aloy-Prosper A, Cervera-Ballester J, et al. Implant treatment in atrophic posterior mandibles: vertical regeneration with block bone grafts versus implants with 5.5-mm intrabony length. Int J Oral Maxillofac Implants. 2014;29(3):659-666.
2. Urban IA, Nagursky H, Lozada JL. Horizontal ridge augmentation with a resorbable membrane and particulated autogenous bone with or without anorganic bovine bone-derived mineral: a prospective case series in 22 patients. Int J Oral Maxillofac Implants. 2011;26(2):404-414.
3. von Arx T, Buser D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: a clinical study with 42 patients. Clin Oral Implants Res. 2006;17(4):359-366.
4. Pieri F, Corinaldesi G, Fini M, et al. Alveolar ridge augmentation with titanium mesh and a combination of autogenous bone and anorganic bovine bone: a 2-year prospective study. J Periodontol. 2008;79(11):2093-2103.
5. Merli M, Lombardini F, Esposito M. Vertical ridge augmentation with autogenous bone grafts 3 years after loading: resorbable barriers versus titanium-reinforced barriers. A randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2010;25(4):801-807.
6. Martínez-Rodríguez N, Barona-Dorado C, Cortés-Breton Brinkmann J, et al. Clinical and radiographic evaluation of implants placed by means of inferior alveolar nerve lateralization: a 5-year follow-up study. Clin Oral Implants Res. 2018;29(7):779-784.
7. Felice P, Pellegrino G, Checchi L, et al Vertical augmentation with interpositional blocks of anorganic bovine bone vs. 7-mm-long implants in posterior mandibles: 1-year results of a randomized clinical trial. Clin Oral Implants Res. 2010;21(12):1394-1403.
8. Bormann KH, Suarez-Cunqueiro MM, von See C, et al. Sandwich osteotomy for vertical and transversal augmentation of the posterior mandible. Int J Oral Maxillofac Surg. 2010;39(6):554-560.
9. Kamperos G, Zografos I, Tzermpos F, Iatrou I. Segmental sandwich osteotomy of the posterior mandible in pre-implant surgery - a systematic review. Med Oral Patol Oral Cir Bucal. 2017;22(1):e132-e141.
10. Dahlin C, Simion M, Hatano N. Long-term follow-up on soft and hard tissue levels following guided bone regeneration treatment in combination with a xenogeneic filling material: a 5-year prospective clinical study. Clin Implant Dent Relat Res. 2010;12(4):263-270.
11. Anitua E, Orive G. Short implants in maxillae and mandibles: a retrospective study with 1 to 8 years of follow-up. J Periodontol. 2010;81(6):819-826.
12. Tawil G, Younan R. Clinical evaluation of short, machined-surface implants followed for 12 to 92 months. Int J Oral Maxillofac Implants. 2003;18(6):894-901.
13. Slotte C, Grønningsaeter A, Halmøy AM, et al. Four-millimeter implants supporting fixed partial dental prostheses in the severely resorbed posterior mandible: two-year results. Clin Implant Dent Relat Res. 2012;14 suppl 1:e46-e58.
14. Kieser JA, Paulin M, Law B. Intrabony course of the inferior alveolar nerve in the edentulous mandible. Clin Anat. 2004;17(2):107-111.
15. Daróz SR, Cardoso ES, Manso MC, Vidigal GM Jr. Evaluation of bone width lateral to the mandibular canal as an alternative approach for implant installation. Implant Dent. 2013;22(1):97-101.
16. Cassetta M, Stefanelli LV, Giansanti M, Calasso S. Accuracy of implant placement with a stereolithographic surgical template. Int J Oral Maxillofac Implants. 2012;27(3):655-663.
17. Ozan O, Turkyilmaz I, Ersoy AE, et al. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 2009;67(2):394-401.
18. Farley NE, Kennedy K, McGlumphy EA, Clelland NL. Split-mouth comparison of the accuracy of computer-generated and conventional surgical guides. Int J Oral Maxillofac Implants. 2013;28(2):563-572.
19. Valente F, Schiroli G, Sbrenna A. Accuracy of computer-aided oral implant surgery: a clinical and radiographic study. Int J Oral Maxillofac Implants. 2009;24(2):234-242.
20. Tahmaseb A, Wismeijer D, Coucke W, Derksen W Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2014;29 suppl:25-42.
21. Pozzi A, Tallarico M, Marchetti M, et al. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur J Oral Implantol. 2014;7(3):229-242.
22. Block MS, Emery RW, Lank K, Ryan J. Implant placement accuracy using dynamic navigation. Int J Oral Maxillofac Implants. 2017;32(1):92-99.
23. Casap N, Wexler A, Persky N, et al. Navigation surgery for dental implants: assessment of accuracy of the image guided implantology system. J Oral Maxillofac Surg. 2004;62(9 suppl 2):116-119.
24. Kim BS, Kim YK, Yun PY, et al. Evaluation of peri-implant tissue response according to the presence of keratinized mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(3):e24-e28.
25. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
26. Linkevicius T, Puisys A, Linkeviciene L, et al. Crestal bone stability around implants with horizontally matching connection after soft tissue thickening: a prospective clinical trial. Clin Implant Dent Relat Res. 2015;17(3):497-508.
27. Chung DM, Oh TJ, Shotwell JL, et al. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006;77(8):1410-1420.
28. Roos-Jansåker AM, Renvert H, Lindahl C, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part III: factors associated with peri-implant lesions. J Clin Periodontol. 2006;33(4):296-301.
29. Schrott AR, Jimenez M, Hwang JW, et al. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20(10):1170-1177.
30. Bengazi F, Wennström JL, Lekholm U. Recession of the soft tissue margin at oral implants. A 2-year longitudinal prospective study. Clin Oral Implants Res. 1996;7(4):303-310.
31. Bouri A Jr, Bissada N, Al-Zahrani MS, et al. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. 2008;23(2):323-326.
32. Flanagan D. Osseous remodeling around dental implants. J Oral Implantol. 2019;45(3):239-246.