Glass-Ionomer Cements: History and Current Status
Since the 1970s, tooth-colored dental restorative materials have taken over as the chief direct dental repair materials. Resin-based composites (RBC) that are bonded to tooth structure by the acid-etch method have been greatly improved in the last 40 years, so that they are now known as the best direct-application enamel replacement materials ever. Today's dentists use these filled resin systems for anterior and posterior tooth restoration with great success.
Another category of tooth-colored dental restorative materials also had its beginnings in the 1970s. Glass-ionomer systems have certain properties that make them the best direct-application dentin replacement repair materials in dentistry. In addition, continuing progress in chemically cured glass-ionomer systems and light-hardened resin-modified glass-ionomers has made certain materials useful for combined dentin and enamel repair. As manufacturers have improved the glass-ionomer systems, more and more dentists are incorporating them into their practices.
The ideal tooth-colored dental restorative material would be a perfect combination of hydrophobic (water-resisting) resin-based composites, with hydrophilic (water-incorporating) glass-ionomers. Such a material would have all the advantages of both systems and avoid the disadvantages. Scientists who develop dental products have made much headway in improving tooth-colored bonded adhesive materials, although the perfect substance to repair teeth has not yet been formulated.
The following article, which serves as a general review of glass-ionomer materials, was written by a dental materials research scientist (Dr. Nicholson) and a pediatric dentist who has used glass-ionomer tooth repair systems routinely in his office since the early 1980s (Dr. Croll). By understanding the scientific basis for development and formulation of glass-ionomer systems, along with how dentists use these materials, dental assistants are valuable partners in providing the best and most advanced clinical dental care for today's patients.
Glass polyalkenoate cements, more commonly known as glass-ionomers, are made of calcium or strontium alumino-fluoro-silicate glass powder (base) combined with a water-soluble polymer (acid). Glass-ionomers were invented in 1969 and reported by Wilson and Kent in the early 1970s.1,2 Glass-ionomer cement components, when blended together, undergo a hardening reaction that involves neutralization of the acid groups by the powdered glass base. Significant amounts of fluoride ions are released during this reaction. Two variations of true glass-ionomer materials that were developed in the 1980s and 1990s are those modified by inclusion of metal and those with a light-polymerized liquid resin component that renders the cement photocurable as part of the overall hardening reaction. The latter are referred to as resin-modified glass-ionomer cements.
The original glass-ionomer commercial formulations introduced in the 1970s failed to gain widespread interest, especially by dentists in North America. Those materials had long setting times, were susceptible to dissolution and desiccation during hardening, and had poor wear resistance and low fracture strengths once set. Regardless of the advantages of fluoride ion release and uptake by enamel and dentin, coefficients of thermal expansion similar to that of tooth structure, chemical bonding to both enamel and dentin, tooth color replication, and biocompatibility, dentists did not readily adopt materials that were difficult to handle and unreliable in the long term.
Classification of Glass-Ionomer Materials
Glass-ionomer cements can be categorized as restorative cements, including liner/base materials, or luting cements. Restorative cements can be further described as self-hardening or partially light-hardening, metal-modified, and resin-modified.
Glass-ionomer luting cements are self-hardening and some are modified with resin. In addition, there are some instances in which a photocurable resin-modified glass-ionomer restorative cement can be used with a lower powder/liquid ratio, to serve as a luting cement. Such material is ideal for cementing orthodontic bands and space maintainers.
In the 1980s, with the goal of creating stronger and more durable glass-ionomer materials, one manufacturer added silver amalgam powder to the glass powder. Another combined the glass powder with elemental silver (cermet) by a process of high-heat fusion.3 The addition of silver had the advantage of increasing radiopacity of the cements. In addition, the wear resistance of the silver cermet cement was somewhat improved over traditional glass-ionomer restorative materials. However, the fracture resistance and fracture toughness of the metal-modified materials proved to be too low to recommend the materials for stress-bearing regions of teeth and the gray color precludes routine use of the cermet in anterior teeth.
Resin-Modified Glass-Ionomer Restorative Cements
A major advancement in glass-ionomer technology was the development of the resin-modified glass-ionomer systems. Vitrebond™ (3M ESPE, www.3mespe.com), a resin-modified glass-ionomer base/liner, was introduced in the late 1980s.4-6 Vitrebond is supplied in a powder/liquid format. A newer version is provided in a paste/liquid system. The polyacid component includes a photopolymerizable resin that hardens the material substantially with visible light exposure. Once the resin component has been cured, the glass-ionomer hardening reaction continues, protected from moisture and overdrying, by the hard resin framework. Rapid "on-command" light-hardening makes the various resin-modified glass-ionomer dentin replacement liner/base materials especially practical to use. GC America (www.gcamerica.com) also makes a resin-modified glass-ionomer base/liner, GC Fuji Lining™ LC. These materials are known for preventing postoperative tooth sensitivity when placed under direct-application resin-based composite restorations, protecting against bacterial access to dentinal tubules, internal fluoride ion release, and antimicrobial action.7-9
Light-hardened resin-modified glass-ionomer restorative cements were introduced in the early 1990s. Some were provided in pre-dosed disposable capsules and others in powder/liquid form, to be spatulated for blending by hand. Like the liner/bases, the resin-modified glass-ionomer restorative cements harden initially by free radical photopolymerization of the resin component. Visible light beam exposure substantially hardens these cements initially and a chemical resin polymerization reaction and the glass-ionomer setting reaction subsequently progress. Addition of the resin component within the glass-ionomer formula not only decreases initial hardening time and handling difficulties, but substantially increases wear resistance and physical strengths of the cement.10,11
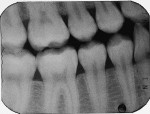
Fracture toughness, fracture resistance, and resistance to wear are all improved in the resin-modified glass-ionomers. In addition, the major advantages of glass-ionomers (fluoride ion hydrodynamics, biocompatibility, favorable thermal expansion and contraction properties, physiochemical bonding to tooth structure) are retained. Clinical reports and clinical research articles after 1993 have reported and documented much success with resin-modified glass-ionomer systems.12-18 Examples of resin-modified glass-ionomer primary and permanent molar repair are shown in Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6.
Fluoride Ion Release and Uptake
With the importance of fluoride in preventive dentistry, glass-ionomer cement systems can be considered therapeutic materials. Fluoride ions are not only released by glass ionomers, but are also taken up by associated enamel and dentin, rendering those tooth structures less susceptible to acid challenge by a combination of decreased solubility and disruption of bacterial activity that produces organic acids.4,7,8,19,20-31 Glass-ionomer materials have been shown to be able to release fluoride at a sustained rate for long periods of time (at least 5 years).20 Also, as water-based systems, they act as continuing fluoride ion reservoirs in the mouth by taking in salivary fluoride from dentifrices, mouthwashes, and topical fluoride solutions at the dental office.32 Fluoride ion dynamics is particularly advantageous for those with high susceptibility to dental caries.
Glass-Ionomer Luting Cements
Early glass-ionomer luting cements were commercially more successful than their restorative counterparts. Their physical strengths were sufficient for cementing stainless-steel crowns, space maintainers, and individual stainless-steel orthodontic bands, and the added benefit of fluoride-ion transfer was an attractive advantage for caries-prone orthodontic patients. Inclusion of the resin component substantially improved the physical properties of glass-ionomer luting cements, and they have since become the standard in prosthodontic and orthodontic applications.
Dentists treating children and orthodontic patients find photopolymerized resin-modified glass-ionomer luting cements especially useful for orthodontic bands and stainless-steel crown cementation.33 The curing light beam is directed on the occlusal surface of the tooth, radiates through tooth structure, and hardens the cement between the band and axial tooth surfaces. Light-hardening the luting cement in this manner takes minutes off the time required to cement each stainless-steel band. In addition, the cement has high physical strengths and is virtually insoluble, so band loosening is uncommon.
Glass-Ionomer/Resin-Based Composite Stratification
Since McLean and Wilson first suggested individualized dentin and enamel repair in combination, there has been much advocacy for the concept.34-40 Tissue-specific tooth restoration by directly overlaying bonded materials has become known as "sandwiching," "layering," or "stratification."
Development of the light-hardened glass-ionomer system has made the placement of a glass-ionomer liner/base much easier and quicker and, therefore, more practical. Based on principles of "biomimesis" (the replacement of tissue, or a part, using materials that most closely replicate the original essence),40,41 it can be argued that the properties of certain glass-ionomer cements make them the best dentin-replacement material currently available, and the resin-based composites are the best enamel substitute.
When used in combination, the original form, function, and appearance of a tooth can be simulated for the long term. Class I resin-based composite with an underlying resin-modified glass-ionomer base is shown in cross-section in Figure 7.
Recent Developments In Glass-Ionomer Systems
Clinical research is producing scientific evidence that resin-modified glass-ionomer cement systems are durable and reliable when used within their limitations in primary and permanent teeth.15,16,18 One might believe that self-hardening glass-ionomer restorative cements are now impractical in comparison to their light-hardened counterparts. However, encapsulated glass-ionomer restorative cements have been introduced that harden by the conventional acid/base neutralization reaction, but have much-improved physical properties compared to any other self-hardening glass-ionomer restorative cement.42
GC Fuji IX GP EXTRA (GC America) and Ketac™ Molar Quick Aplicap™ (3M ESPE) both have a rapid set, which significantly reduces early moisture sensitivity. Faster hardening has been achieved by altering the particle size and particle size distribution of the glass powder. Such materials are ideal for certain uses in primary teeth; interim restorations in permanent teeth; long-term, non-stress-bearing restorations in permanent teeth, and in the atraumatic restorative technique (ART).
ART has gained much interest internationally for patient populations who lack the advantages of modern dentistry.43 GC America has produced GC Fuji TRIAGE, a self-hardening glass-ionomer sealant and surface protective material that is particularly useful for erupting permanent first and second molars with partially exposed grooves that are not yet able to be sealed with conventional resin sealant.
The latest advancement in glass ionomers is the "nano-ionomer." Ketac Nano™ (3M ESPE) is a resin-modified glass-ionomer restorative cement that was introduced in 2007. A double-barreled "clicker" exudes correct portions of two pastes to be blended by spatulation. According to the manufacturer, Paste A is resin-based and contains fluoroaluminosilicate glass, silane-treated silica and zirconia-silica nanofillers, methacrylate and dimethacrylate resins, and photoinitiators. Paste B is water-based and contains polyalkenoic acid copolymer (Vitrebond Copolymer), silane-treated zirconia-silzica nanoclusters, silane-treated silica nanofiller, and hydroxymethylmethacrylate (HEMA). Ketac Nano Primer contains water, HEMA, polyalkenoic-acid copolymer, and photoinitiators.
The glass filler formulation of this nano-ionomer makes for a resin-modified glass-ionomer material with high polishability, enhanced tooth shade-matching potential, and better physical properties.44,45 All other properties of glass-ionomer systems are retained. Ketac Nano restorative cement is recommended for primary teeth restorations, interim repair of all permanent teeth, relatively confined Class I restorations, Class III and Class V tooth repair, and certain core build-ups. Examples of nano-ionomer tooth repair are shown in Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13, Figure 14, Figure 15, Figure 16, Figure 17, Figure 18 and Figure 19.
Conclusion
In the last 20 years, dental materials scientists have worked diligently to produce glass-ionomer cement systems that overcome the three chief disadvantages of this class of materials: difficult handling properties, poor resistance to surface wear, and poor resistance to fracture. They have produced products that are so improved that these major disadvantages have been significantly reduced. Such improvements are bound to continue and glass-ionomer cement formulations will gain even more importance in restorative dentistry, preventive dentistry, and orthodontics.
Disclosure
The authors have no financial interest in any products or manufacturers mentioned in this article.
Acknowledgment
Much of the text of this article was adapted from: Croll TP, Nicholson JW. Glass-ionomer cements in pediatric dentistry: review of the literature. Pediatric Dentistry. 2002;24(5):423-429. Used with permission.
References
1. Wilson AD, Kent BE. The glass-ionomer cement: a new translucent dental filling material. J Appl Chem Biotechnol. 1971;21:313.
2. Wilson AD, Kent BE. A new translucent cement for dentistry: The glass ionomer cement. Brit Dent J. 1972;132(4):133-135.
3. McLean JW, Gasser O. Glass-cermet cements. Quintessence Int. 1985;16(5):333-343.
4. Mitra SB, Creo AL. Fluoride release from light-cure and self-cure glass ionomers. J Dent Res. 1989;68:274 [Abstract #739].
5. Mitra SB. Property comparisons of a light-cure and a self-cure glass ionomer liner. J Dent Res. 1989;68:274 [Abstract #740].
6. Mitra SB. Adhesion to dentin and physical properties of a light-cured glass-ionomer liner/base. J Dent Res. 1991;70(1):72-74.
7. Tam LE, Chan GP, Yim D. In vitro caries inhibition effects by conventional and resin-modified glass-ionomer restorations. Oper Dent. 1997;22(1):4-14.
8. Scherer W, Lippman N, Kalm J, LoPresti J. Antimicrobial properties of VLC liners. J Esthet Dent. 1990;2(2):31-32.
9. Shelburne CE, Gleason RM, Mitra SB. Measurement of microbial growth inhibition and adherence by glass ionomers. J Dent Res. 1997;76:40 [Abstract 211].
10. Mitra SB, Kedrowski BL. Long-term mechanical properties of glass ionomers. Dent Mater. 1994;10(2):78-82.
11. Douglas WH, Lin CP. Strength of the new systems. In: Hunt PR ed. Glass Ionomers: The Next Generation. (Proceedings of the 2nd International Symposium on Glass Ionomers) Philadelphia: International Symposia in Dentistry; 1994: 209-216.
12. Croll TP, Killian CM, Helpin ML. A restorative dentistry renaissance for children: Light-hardened glass ionomer/resin cement. ASDC J Dent Child. 1993;60(2):89-94.
13. Croll TP, Helpin ML. Class II Vitremer restoration of primary molars. ASDC J Dent Child. 1995;62(1):17-21.
14. Uno S, Finger WJ, Fritz U. Long-term mechanical characteristics of resin-modified glass ionomer restorative materials. Dent Mater. 1996;12(1):64-69.
15. Donly KJ, Kanellis M, Segura A. Glass ionomer restorations in primary molars: 3-year clinical results. J Dent Res. 1997;76:41 [Special Issue, Abstract #223].
16. Donly KJ, Segura A, Kanellis M, Erickson RC. Clinical performance and caries inhibition of resin-modified glass ionomer cement and amalgam restorations. J Amer Dent Assoc. 1999;130:1459-1466.
17. Croll TP, Helpin ML, Donly KJ. Vitremer restorative cement for children: three clinicians' observations in three pediatric dental practices. J Dent Child. 2000;67(6):391-398.
18. Croll TP, Bar-Zion Y, Segura A, Donly KJ. Clinical performance of resin-modified glass ionomer cement restorations in primary teeth. A retrospective evaluation. J Amer Dent Assoc. 2001;132:1110-1116.
19. Ewoldsen N, Herwig L. Decay-inhibiting restorative materials: past and present. Compend Cont Educ Dent. 1998;19(10):981-992.
20. Forsten L. Fluoride release and uptake by glass-ionomers and related materials and its clinical effect. Biomaterials. 1998;19(6):503-508.
21. Swartz ML, Phillips RW, Clark HE. Long-term fluoride release from glass ionomer cements. J Dent Res. 1984;63(2):158-160.
22. Hicks MJ, Flaitz CM, Silverstone LM. Secondary caries formation in vitro around glass ionomer restorative materials. Quintessence Int. 1986;17:527-532.
23. Griffin F, Donly KJ, Erickson RC. Caries inhibition of three fluoride-releasing liners. Am J Dent. 1992;5:293-295.
24. Donly KJ: Enamel and dentin demineralization inhibition of fluoride-releasing materials. Am J Dent. 1994;7:275-278.
25. Souto M, Donly KJ. Caries inhibition of glass ionomers. Am J Dent. 1994;7(2):122-124.
26. Forsten L. Resin-modified glass ionomer cements: Fluoride release and uptake. Acta Odontol Scand. 1995;53(4):222-225.
27. Donly KJ, Ingram C: An in vitro caries inhibition of photopolymerized glass ionomer liners. J Dent Child. 1997;64:128-130.
28. Segura A, Donly KJ, Stratmann R. Enamel remineralization of teeth adjacent to Class II glass ionomer restorations. Am J Dent. 1997;10(5):247-250.
29. Donly KJ, Segura A, Wefel JS, Hogan MM. Evaluating the effects of fluoride-releasing dental materials on adjacent interproximal caries. J Am Dent Assoc. 1999;130:817-825.
30. Jang KT, Garcia-Godoy F, Donly KJ, Segura A. Remineralizing effects of glass ionomer restorations on adjacent interproximal caries. ASDC J Dent Child. 2001;68(2):125-128.
31. Marinelli CB, Donly KJ, Wefel JS, et al. An in vitro comparison of three fluoride regimens on enamel remineralization. Caries Res. 1997;31(6):418-422.
32. Donly KJ, Nelson JJ. Fluoride release of restorative materials exposed to a fluoridated dentifrice. ASDC J Dent Child. 1997;64(4):249-250.
33. Croll TP, Helpin ML. Space maintainer cementation using light-hardened glass ionomer/resin restorative cement. J Dent Child. 1994;61:246-248.
34. McLean JW, Wilson AD. The clinical development of the glass-ionomer cement. II. Some clinical applications. Aust Dent J. 1977;22(2):120-127.
35. McLean JW, Powis DR, Prosser HJ, Wilson AD. The use of glass-ionomer cements in bonding composite resins to dentine. Br Dent J. 1985;158(11):410-414.
36. Mount GJ. Clinical requirements for a successful ‘sandwich'—dentine to glass ionomer cement to composite resin. Aust Dent J. 1989;34(3):259-265.
37. Croll TP. Replacement of defective class I amalgam restoration with stratified glass ionomer-composite resin materials. Quintessence Int. 1989;20:711-716.38. Davidson CL. Glass-ionomer bases under posterior composites. J Esthet Dent. 1994;6(5):223-224.
39. Ferrari M. Use of glass-ionomers as bondings, linings, or bases. In: Davidson CL, Mjor IA, eds. Advances in Glass-Ionomer Cements. Berlin/Chicago: Quintessence Publishing Co, 1999:137-148.
40. Croll TP, Cavanaugh RR. Posterior resin-based composite restorations: a second opinion. J Esthet Restor Dent. 2002;14(5):303-312.
41. Bugliarello G. Biomimesis. The road less traveled. The Bridge. 1997;27(3):2-3.
42. Croll TP. Rapid setting, encapsulated glass-ionomer restorative cement. Compend Cont Educ Dent. 2001;22:442-448.
43. Smales RJ, Yip HK. The atraumatic restorative treatment (ART) approach for primary teeth: review of literature. Pediatr Dent. 2000;22:294-298.
44. Croll TP, Berg JH. Resin-modified glass-ionomer restoration of primary molars with proximating Class II caries lesions. Compend Cont Educ Dent. 2007;28:372-377.
45. Croll TP. Nanofilled resin-modified glass ionomer restorative cement. Contemporary Esthetics. 2007;11:14-17.
46. Croll TP. Lateral access Class II restoration using resin-modified glass ionomer or silver cermet cement. Quintessence Int. 1995;26:121-126.
About the Authors
Theodore P. Croll, DDS
Private Practice, Pediatric Dentistry
Doylestown, Pennsylvania
Adjunct Professor
Pediatric Dentistry
University of Texas Health Science Center at San Antonio
San Antonio, Texas
John W. Nicholson, PhD
Professor of Biomaterials Chemistry
Department of Chemical, Environmental and Pharmaceutical Sciences, School of Science
University of Greenwich, Medway Campus
Chatham, Kent, United Kingdom